Is spinal flexion actually dangerous when squatting or deadlifting?
You’ve probably been taught to keep your spine and pelvis in a relatively neutral position while squatting or deadlifting. Specifically, you’re not supposed to let your back round over (spinal flexion) or allow ‘butt wink’ (posterior pelvic tilt), lest you injure your back. The idea that rounding your back under high loads increases injury risk was regarded as proven beyond doubt, almost self-evident. But is it true? If you’ve been following my work for a while, you’ve seen many popular ideas get debunked. In fact, if you’ve been following some of the modern physiotherapists and pain science experts, you may have seen that this idea is now regarded as completely debunked in many circles. The very idea of an injurious exercise is in some circles regarded as a fallacy. Are Starting Strength and all the common textbooks about how to squat and deadlift wrong? Let’s see what the research says about spinal flexion and injury risk.
Why spinal flexion may be injurious
The theory that spinal flexion can injure the spine was chiefly popularized by Stuart McGill, but is shared by many other researchers. It’s the most widely recommended lifting technique in scientific research. The argument goes like this. When the spine is in a neutral, anatomical position, such as when you’re standing upright, the spine is very sturdy. In anatomical or neutral position, the strain on the passive structures of the spine is minimal and compressive forces going down the spine are quite well-tolerated. The risk seems to increase dramatically when we flex the spine. Spinal flexion in the lumbar region – such as when letting your lower back round over during squats or deadlifts – exponentially increases shearing stress on the spine, and this significantly reduces the load required to injure a disc [2, 3, 4]. The greater the spinal flexion, the fewer spinal extension repetitions are required to injure a disc. This model of back injury also explains why most disc herniations in lifters protrude to the back of the body, rarely the front. Spinal flexion essentially pushes out the disc to the back.
Thus, it’s safest to keep the spine in the neutral range as much as possible when squatting or deadlifting to minimize spinal shearing stresses and their resulting injury risk. Use your legs as much as possible and try to keep your spine rigid in its neutral position when lifting heavy objects.
The case against loaded spinal flexion is very plausible, but it has come under scrutiny for various reasons.
Absence of evidence
The first and foremost argument against the traditional view on spinal flexion relates to the quality of the evidence. If you check the papers I cited, you’ll see most of the supporting research is from modeling, animal and human cadaver studies. We don’t have any studies that compare lifters squatting or deadlifting appreciable weights with a neutral vs. flexed spine and measuring how often they get injured with either technique. In this sense, you could argue for the null hypothesis that since there’s no direct evidence for or against lifting with a neutral spine, you can do whatever you want. However, this is mistaking absence of evidence for evidence of absence. Plus, there are actually 2 notable papers in living humans that support the theory that spinal flexion is risky.
A randomized, controlled trial by Suni et al. (2013) found that back movement training, including in particular the avoidance of full lumbar flexion, reduced lower back pain in military personnel.
An 18-month randomized, controlled trial by Snook et al. (1998) found that instructing patients with non-specific back pain not to flex their spines in the mornings led to significantly faster recovery of pain and disability than a sham control intervention.
Without more hard data in strength training humans, I think it makes sense to go with the data and theory that we do have. The main theory itself has also been criticized, however.
Refutation of greater stresses in flexion?
While we don’t have good studies measuring spinal forces in serious strength trainees lifting with various techniques, we do have such data in untrained individuals and manual laborers. These data are very imperfect for our purposes, as most studies are on untrained subjects lifting light objects, often from the floor, with very different techniques than you’d use to deadlift or squat a barbell. Crucially, it’s virtually impossible to pick up an object like a moving box from the floor without rounding the spine, so the ‘good technique’ in many studies does not actually entail a neutral spine. Then again, at least we’re looking at living humans. And the data in living humans do not neatly support the theory that rounding of the back increases the total stress on the spine. However, this is unsurprising given the multitude of limitations of such research and, importantly, a good deal of research does in fact find that keeping the spine neutral minimizes internal spinal loads. To my knowledge, the latest meta-analysis comparing different lifting techniques on spinal loads is from 1999, but it found lifting while bending over from the spine (Stoop lifting) increases shearing forces on the spine without majorly affecting compressive forces or net moments compared to squat lifting.
Thus, the research measuring spinal forces in living humans is overall in line with the modeling, animal and human cadaver research popularized by Stu McGill. Keeping the spine in the neutral range seems to minimize spinal loading, in particular shearing forces, as biomechanically expected.
You can’t actually prevent the spine from moving when squatting or deadlifting
It may look like you can, but you can’t. Almost nobody will be able to keep their spine and pelvis in perfectly anatomical position while lifting, not even powerlifters or Olympic weightlifters. Some spinal flexion occurs even when you focus on trying to minimize spinal movement and no movement may be visible from the outside [2, 3]. One study reported that a pelvic tilt over 36° is required for physical therapists to accurately identify it in weightlifters, and the physical therapists were overall poor at detecting pelvic and spinal motion.
Some people have taken these findings to mean that “Ha! You can’t actually keep your spine straight, so you shouldn’t try.” However, this is a strawman argument. The traditional advice to lift with a straight back does not literally require zero movement in the spinal joints. It’s not necessary and probably even counterproductive to try to lift with absolutely zero lumbopelvic movement, because the neutral ‘position’ of the spine where passive structures are under minimal strain is actually a neutral range with around 2-20° lumbar spinal flexion-extension range of motion. And it’s not like you’ll pop a disc the moment you venture out of this range. The traditional theory says the risk increases the further out from the neutral range you go. The risk also obviously increases with training volume, intensity and duration. There’s a certain amount of stress that your spine will withstand for a certain period of time. The greater the spinal flexion, the fewer spinal extension repetitions are required to injure a disc. Most research finds that weightlifters and Powerlifters have their spine go a bit beyond the neutral range while lifting, but they stay pretty close to it and rarely go into end range of motion. In fact, in one study, a powerlifter reported low back discomfort precisely when he exceeded maximal lumbar flexion range of motion during the deadlift.
Questionable effectiveness in manual laborers
Another line of research that’s been brought up to debunk traditional lifting technique is from manual laborers, such as factory workers. Many studies have found no effect on injury rates of coaching manual laborers to lift with a straight back. A 2020 review of the effectiveness of teaching manual laborers to lift from the legs with a straight back found that only about half of all studies report positive effects and only a quarter report a reduction in injury rates. However, there are virtually no studies reporting harmful effects of lifting with a straight back, so the overall body of evidence still favors lifting with a neutral spine. For example, a randomized controlled trial by Loisel et al. (1997) found that ergonomic counseling of manual laborers with back pain was significantly and considerably more effective to facilitate return to work than usual care from a physician. Importantly, ergonomic counseling had additive effects to clinical intervention with possible physical and cognitive behavioral therapy. A secondary subgroup analysis by Loisel et al. (1997) of the same dataset looked at nurses with back pain from heavy shifts. The researchers compared nurses with vs. without core training designed to teach them how to keep their spine neutral (much like the McGill method). The nurses doing core training achieved a greater reduction in pain.
How come some studies have such clear results whereas others don’t? The lower than theoretically expected effectiveness of some of the programs may in large part be due to workers’ non-compliance with the recommended lifting technique. Lifting purely from the legs requires more effort than involving the back as well and it’s not even possible in the first place for many tasks, such as lifting boxes from the floor. I know many people in general who have been taught to lift objects with their legs instead of their backs, but very few people actually do it.
So overall, the data on injury rates in manual laborers again lean in the direction of keeping the spine straight while lifting to prevent back injuries.
Pain science
Another line of research casting doubt on the ‘lumbar flexion is risky’ argument comes from pain sciences. Pain science has become much more mainstream over the past decade and in some circles has caused a massive paradigm shift. Here’s the short version.
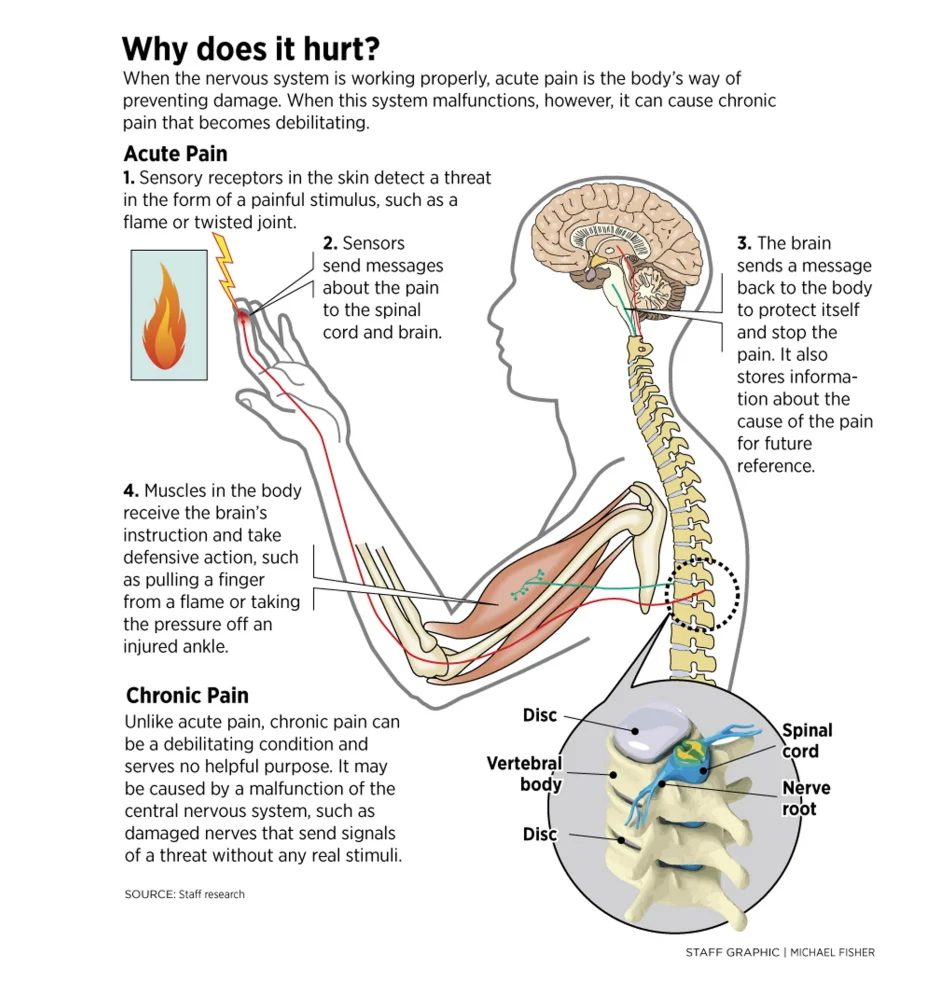
Intuitively, many people think of pain as a warning about tissue damage. Pain is an evolutionary mechanism to cease potentially harmful activities. Pain says ‘stop’. Pain does not always correlate with tissue damage, however. Pain is biopsychosocial, meaning the experience of pain is a combination of biological (e.g. tissue damage), psychological (e.g. nocebo effects) and social effects (e.g. not wanting to show pain). Pain is triggered by pain receptors (nociceptors) in the nervous system and ultimately, it’s the brain that decides whether you experience pain. Pain receptor activation does not always correspond to physical tissue damage. You can have pain in the absence of injury. You can also be injured without damage to nerves or with complete destruction of the nerves so you don’t feel the damage. You can even experience pain in body parts you no longer have after extreme trauma or surgery (phantom limb pain). The following graphic summarizes how we experience pain.
Some types of pain have surprisingly little to do with injury to the body and are essentially psychogenic (’caused by the psyche’), a nocebo effect: you get pain, because you expect pain. This type of pain is often related to stress and anxiety. This type of pain is not as rare as you may think. In fact, most chronic back pain without a clear acute onset – an ‘oh, crap’ moment – seems to be psychosomatic rather than mechanical. In contrast to popular belief, daily life posture, back strength and muscle length have very little relation to back pain [2, 3, 4, 5, 6, 7, 8] outside of pathological weakness. It takes a lot of force to damage the spine and not a lot of strength or mobility to move it without external loading, so for most people, especially for strength trainees, muscular issues are not plausible culprits.
The knowledge that pain is not a direct indicator of tissue damage but a complex signal with a significant psychological component has spurred a revolution in our understanding of pain. However, I see a lot of people on social media who have run completely wild with the idea that pain is all in our head. These individuals had clearly never studied even the most basic pain science or psychological literature before and now feel like they took the Red Pill and found out everything they thought about musculoskeletal injuries was a lie. That is not the case. If you study people with pain without a plausible biomechanical cause — they were sedentary and cannot tell you exactly when the pain started — it makes sense that there is in fact often no biomechanical cause. Your average physiotherapist gets a lot of these clients, so they may think this is the case for everyone. However, if you work with strength trainees who consistently come to you with back pain that started during a heavy set of deadlifts with a loud pop and is now consistently aggravated by spinal loading, especially in spinal flexion, I hope you can see this is likely indeed a biomechanical injury, not a nocebo.
The pain science revolution has actually taught us very little with relevance for strength trainees with acute musculoskeletal injuries. The effect of cognitive, emotive and behavioral factors on recovery from musculoskeletal injury is modest and insignificant in many scenarios. Under normal circumstances for strength trainees, listening to your body and avoiding pain is a good way to autoregulate your training when you’re injured [2, 3, 4, 5]. For example, Long et al. (2004) evaluated 312 people with back pain for their directional preference: which movements caused pain and which did not, such as spinal flexion vs. extension. The researchers then had the patients perform an exercise program that was either not related to their pain preference, in line with their movement preference or directly opposite their movement preference. The patients that exercised so as to avoid pain improved on every outcome, including a decrease in pain and disability. The patients that did not heed their pain signals for their exercise programs improved around 3-fold less. In fact, a third withdrew from the study within 2 weeks due to worsening or persistence of their symptoms. Even in cases where training through pain can be beneficial for short-term recovery from musculoskeletal injuries, not training through pain provides similar long-term results according to a 2017 meta-analysis, so not training through pain is safer. This is especially true for strength training injuries, as most strength training injuries by far are overuse injuries [2].
Long story short, if squatting or deadlifting starts hurting your back, you should generally take that pain seriously and see if you can get rid of the pain by changing your technique. This brings us to the last important line of evidence.
Observations from the field
Given that there’s virtually no direct research relating exercise technique to injury risk in healthy strength trainees, we should take anecdotal observations more seriously than if we had more research. The experience from the trenches is quite clear in my experience. Most coaches I’ve talked to agree that their clients get injured more often, or at least report pain more often, when squatting or deadlifting with a lot of spinal flexion or butt wink. However, we should always be very skeptical of anecdotal observations and very concretely define our observations, because everyone is susceptible to confirmation bias. After over a decade of coaching strength trainees myself, however, I can say that some observations are pretty compelling. For example, I’ve had many clients that reported squatting or deadlifting gave them back pain. Upon teaching them what I think is good technique, the pain was gone. Multiple also said they tried many times to squat or deadlift, but every time they got injured. Again, they did not get injured anymore (or much more rarely) during the coaching. This could be affected by many other aspects of the coaching, such as better nutrition or a better regulated training volume, but I’ve also seen the effects acutely, including in myself. Many people with back pain feel more pain when squatting or deadlifting with butt wink or spinal flexion. It hurts with visible rounding but feels ok with a more neutral spine. I’ve also seen it in the leg press. After a back injury, I sometimes replace squats with leg presses and some people gloss over the instruction that they should also keep their spine and pelvis reasonably neutral. Not doing so causes pain and correcting this fixes the pain. These are all uncontrolled observations, but they’re consistent and they’re shared by many coaches, so without evidence to the contrary, and with theory to support them, I think we should not completely discard them.
Last but certainly not least, the instructions to lift with a relatively rigid back and pelvis is not just a good potential way to avoid injury but also an effective way to lift. Most high-level powerlifters keep their spines relatively rigid during squats and deadlifts.
Conclusion
Biomechanics teach us that spinal flexion under load, such as during squats and deadlifts, considerably increases shearing stresses on the spine. While this evidence comes mostly — but not exclusively — from cadavers and computer models of the body, the limited data we have on spinal forces in living humans and injury rates in manual laborers tentatively albeit inconsistently align with the biomechanical expectations. The theory also fits with what we see in the field and with how most competitive barbell sports athletes lift: when possible, their spinal and pelvic movement generally stays contained below the threshold of visual detection. Considering there is no notable evidence that lifting like this is harmful, I think the prudent course of action in this case is to lift like the pros and scientists have advocated all along. In general, don’t let your spine flex or your pelvis posteriorly tilt more than necessary when you’re lifting heavy weights.
- For squats, Goodmornings and Romanian deadlifts, it should be realistic to avoid any clearly visible spinal flexion or butt wink.
- For deadlifts from the floor, you face a trade-off. While it may be safest to deadlift like you squat, you’ll be considerably weaker this way. The traditional compromise from powerlifters is to set up with a rounded over upper back (thoracic spine) and a straight lower back (some spinal flexion but not into the end range) and then to maintain that spinal alignment as rigidly as possible during the lift.
That said, some people clearly take the avoidance of spinal flexion too far. Most research does not find relations between daily life postures and lifting techniques with back pain. The loads are too low and the repetitions too few to cause a biomechanical injury under normal circumstances. So you don’t have to go through life like a stiff robot and do a perfect deadlift every time you pick up a pencil.
 Want more content like this?
Want more content like this?
Then get our free mini-course on muscle building, fat loss and strength.
By filling in your details you consent with our privacy policy and the way we handle your personal data.